Enhancing Risk Adjustment Accuracy and Revenue Integrity with AI-Powered HCC Coding
In April, the Centers for Medicare & Medicaid Services (CMS) released its 2026 Medicare Advantage (MA) Rate Announcement, projecting a 5.06% average increase in payments to MA plans. That’s a notable jump from the 3.70% increase we saw in 2025. More than just a financial adjustment, this signals growing confidence in the Medicare Advantage model—and with it, growing expectations.
What does this mean simply? Insurance companies offering these plans will receive more government funding, which can be used to improve care for members, invest in better technology, and stay aligned with stricter requirements for quality and accuracy. In essence, more money equates to better patient care.
At John Snow Labs, we see this as a call to action for both payers and providers to:
- Improve coding accuracy
- Strengthen risk adjustment performance
- Streamline operations through intelligent automation
Our state-of-the-art Hierarchical Condition Category (HCC) coding solution was designed to help healthcare providers and payers improve risk adjustment accuracy and revenue integrity. Built on healthcare-specific LLMs and NLP models, we can help organizations unlock these outcomes within their own environment, trained on their data, all while seamlessly integrated into their existing workflows.
But first, let’s dive into why this matters.
More Than Just a Rate Bump
This higher rate gives plans more flexibility to invest in the areas that matter most. For years, innovation in Medicare Advantage has been held back by tight margins and operational complexity. Now, with more resources at play, plans can accelerate their efforts to modernize operations.
This includes rethinking how to manage risk adjustment, automate coding and chart review processes, and deliver more personalized member experiences. And with CMS reinforcing its requirements for documentation and outcomes, the additional funding comes at a critical time. Because what CMS is doing goes beyond economics—it’s a clear policy signal.
As Medicare Advantage becomes the dominant form of Medicare coverage, the agency is raising the bar. Plans are being pushed to deliver more accurate risk scores, improve coding integrity, and generate actionable insights at the individual member level. In short, they must prove that the MA model can deliver better value, not just broader reach. This shift opens a new window for innovation, especially for healthcare technology companies that can help MA plans rise to the occasion.
HCC Coding Explained
Accurate HCC coding is a critical piece of this puzzle. For patient risk adjustment, it directly impacts reimbursement models and financial sustainability in value-based care. However, studies indicate that as many as half of all patients may have prior conditions, complications, or severity indicators documented in clinical notes but not reflected in claims or electronic health records (EHRs).
This is a problem considering HCC coding impacts:
- How Much Plans Get Paid: Medicare pays MA plans based on how sick their members are—not just how many people they cover, and HCC coding is how plans uncover that information. The more accurately a plan captures and reports chronic illnesses, the more fairly it gets paid to manage member care.
- Member Care: Accurate HCC coding isn’t just about appropriate funds allocation, but ensuring care teams understand a patient’s full clinical history. If important diagnoses are missed or undocumented, gaps in care, missed interventions, or inappropriate treatment plans are more likely.
- Regulatory Compliance: CMS audits MA plans to make sure the diagnoses they submit are actually supported by the patient’s medical records. Poor HCC coding can lead to penalties, lost revenue, or worse.
- Quality and Outcomes: Accurate HCC coding supports broader goals like population health management, care coordination, and value-based care.Understanding your high-risk patients leads to earlier intervention and improved outcomes across the board.
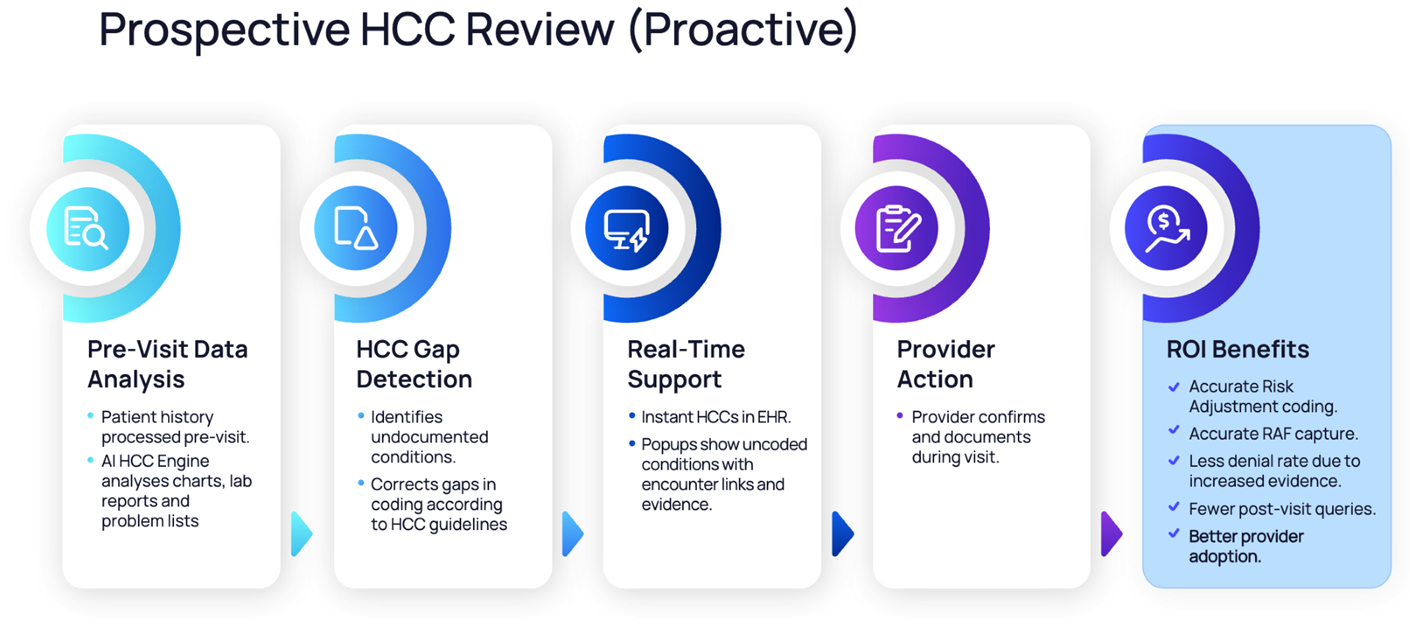
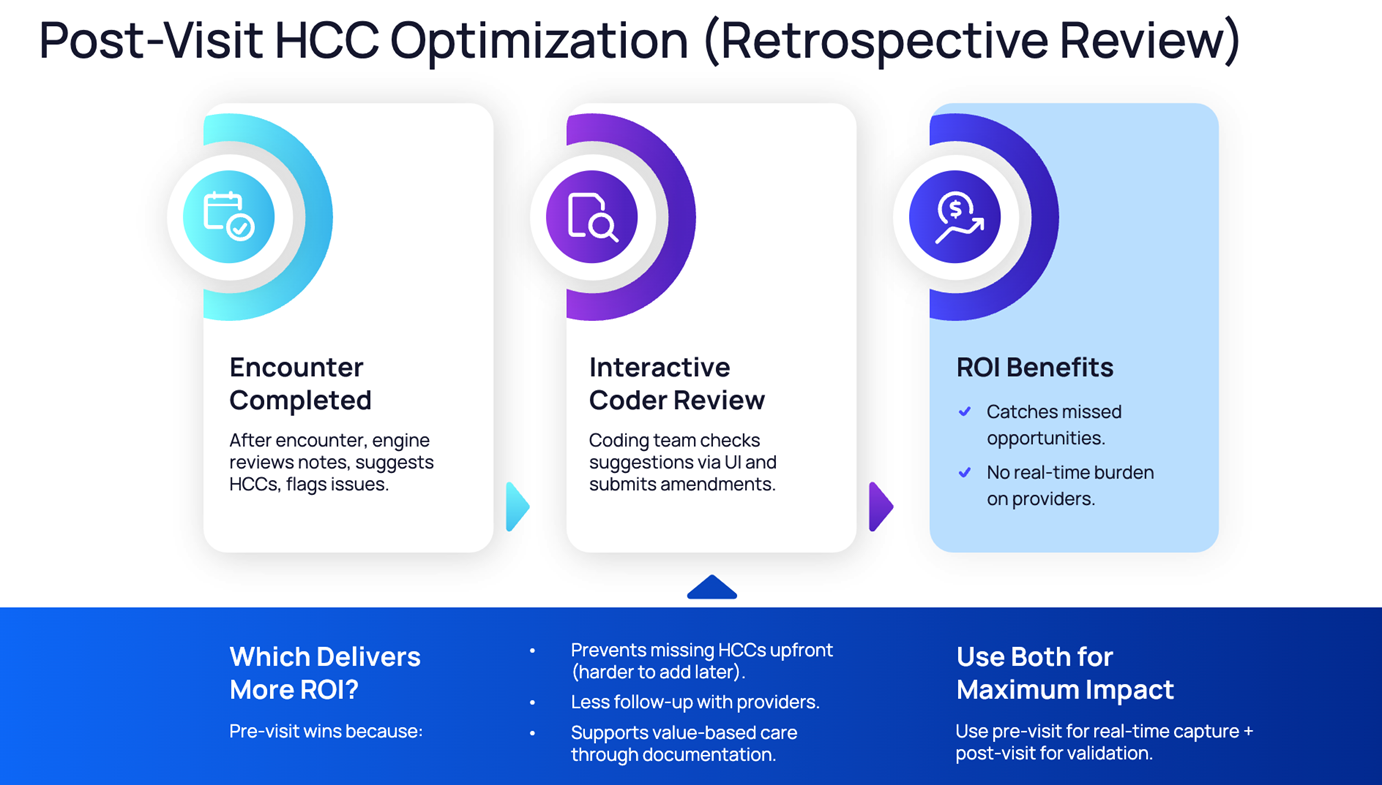
Enabling Transformation with John Snow Labs
At John Snow Labs, we’re helping payers and providers navigate these changes effectively. Powered by state‑of‑the‑art, healthcare‑specific language models, healthcare organizations can bring AI‑powered HCC coding in‑house, empowering clinical teams with greater control, scalability, and cost efficiency. Our technology can enable both prospective and retrospective review.
With strict privacy and customization options, our HCC coding solution operates entirely within a client’s environment, meaning no protected health information (PHI) leaves their firewall. It can also be trained on a plan or provider’s own charts enabling the model to understand their patient population. This dramatically improves the accuracy of condition capture while easing the workload on medical coders.
Additionally, integrating AI into the coding workflow can reduce dependency on outsourced coding services, minimizing coding gaps and improving overall compliance. In other words, it’s an easily implemented solution that meets the unique demands of a healthcare environment.
While John Snow Labs has an existing patient risk adjustment solution to accurately assess and assign HCC codes for precise reimbursement of health insurance plans, these upgrades automate the discovery of missed clinical codes from free-text patient notes. It then prioritizes them based on their impact on risk adjustment scores and provides a human-in-the-loop validation tool for audit and review.
It’s not just automation—it’s a smarter, more contextual approach that aligns directly with reimbursement and documentation goals.
An Opportunity for Innovation
The 2026 Medicare Advantage Rate Announcement isn’t just a higher number. It reflects expectations for the next phase of value-based care and challenges every stakeholder in the MA ecosystem to level up. And for payers and providers willing to invest in the right technologies, it’s an opportunity.
If your organization is reassessing its risk adjustment workflows, looking to streamline operations, or working to better align with the evolving policy landscape, we’re here to help. As Medicare Advantage continues to grow, success will hinge on delivering precision at scale—and that’s exactly what we’re focused on at John Snow Labs.
Read the CMS 2026 Medicare Advantage and Part D Rate Announcement Fact Sheet for more information. To learn more about how we’re helping leading health plans and providers transform risk adjustment, check out a recording of our recent Healthcare NLP Summit session, “Transforming HCC Coding with Healthcare-Specific Language Models.”